For most people living with migraine, painkillers feel like a lifeline. When the pain hits, reaching for a pill is often the fastest and most reliable way to survive the day. Over time, this habit becomes automatic – headache equals medication. But few patients are warned that this very strategy can quietly turn against them.
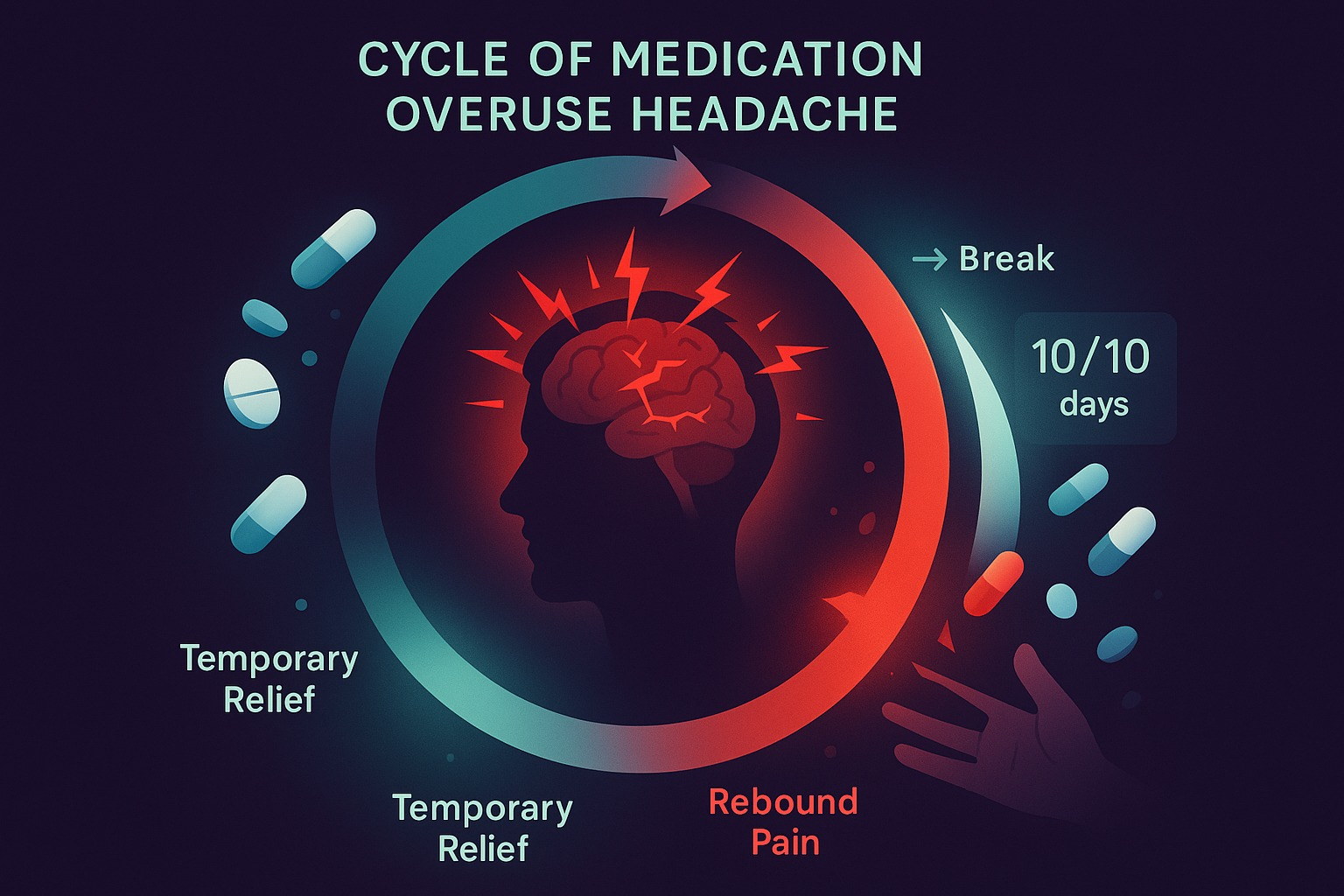
There is a well-documented condition called Medication Overuse Headache (MOH), and it represents one of the most common and misunderstood reasons why episodic migraine slowly turns into a chronic, almost daily problem.
What makes MOH especially dangerous is that it doesn’t feel like a mistake. It feels like responsibility. You take your medication exactly because you want to function, work, care for your family, and avoid suffering. Yet, paradoxically, the brain may begin to depend on the drug itself.
How Medication Overuse Headache Develops
Medication Overuse Headache occurs when the brain is exposed to pain-relieving drugs too frequently. Instead of calming pain pathways, repeated exposure changes how the nervous system processes pain signals.
Over time, the brain becomes hypersensitive. Pain pathways lower their activation threshold, and the absence of medication itself starts to feel like a trigger. This is why many people with MOH wake up with a headache every morning, even before doing anything “wrong.”
Research shows that up to 2% of the global population is affected by MOH, and among people with chronic migraine, the numbers are even higher – up to 30%. In other words, nearly one in three chronic migraine patients may be stuck in a medication-driven cycle without realizing it.
The Dangerous Thresholds Most Patients Never Hear About
One of the biggest problems is that overuse does not require extreme behavior. Many patients cross the line without exceeding prescribed doses.
Science-defined risk thresholds per month are surprisingly low:
-
Triptans – 10 or more days
-
Opioids or combination painkillers – 10 or more days
-
Simple analgesics (such as paracetamol or NSAIDs) – 15 or more days
Once these limits are crossed consistently, the brain may begin reinforcing headache patterns instead of suppressing them.
The cruel irony is that the medication still works temporarily. Pain goes down. Relief happens. And that reinforces the behavior, even while the underlying problem grows stronger.
Why the Cycle Is So Hard to Break
Medication Overuse Headache is not just a behavioral issue – it’s a neurological one. The brain adapts to repeated chemical input. Dopamine, serotonin, and pain modulation systems start expecting the drug.
When intake is reduced or stopped, withdrawal-like symptoms appear: worsening headaches, nausea, anxiety, and fatigue. This is why breaking the cycle often takes 2 to 6 months, even under medical supervision.
Many patients interpret this rebound phase as proof that they “need” the medication. In reality, it’s a sign that the nervous system is recalibrating.
Awareness Is the First Real Treatment
The most effective first step in preventing MOH is not willpower – it is visibility.
Most patients cannot accurately recall how often they take painkillers across weeks or months. Migraine days blur together. Medications taken “just in case” get forgotten. Patterns stay invisible.
This is where structured tracking changes everything.
By logging headache days, medication intake, and timing, patients begin to see something they couldn’t feel before: frequency trends. The moment medication days start clustering, the risk becomes obvious.
That is exactly why tools like https://hopeandmo.com focus on migraine and medication tracking together. When the brain sees the pattern clearly, behavior becomes easier to adjust before crossing dangerous thresholds.
MOH Is Preventable – But Rarely Discussed
Medication Overuse Headache is not a failure of discipline, intelligence, or self-control. It is a predictable neurological response to repeated exposure, and it can happen to anyone.
The real failure lies in education. Too many patients are told what to take, but not how often is too often. By the time daily headaches appear, the cycle is already deeply ingrained.
Understanding MOH early allows patients and clinicians to shift strategies – using preventive treatments, non-pharmacological approaches, and better pacing of rescue medications.
Final Summary: What to Remember
Medication Overuse Headache is one of the most common hidden drivers of chronic migraine. It affects up to 30% of chronic patients and often develops quietly through well-intentioned medication use. The brain adapts to frequent pain relief by lowering its pain threshold, creating a self-sustaining cycle.
The key thresholds are lower than most people expect, and once crossed, recovery can take months. However, MOH is reversible, especially when patterns are identified early.
Tracking medication intake is not about restriction – it’s about awareness. When you can see the cycle, you gain the power to stop it before pain becomes the default state.
Quick question for readers:
Would it help you if an app warned you when you’re approaching medication overuse limits – before headaches become daily?
