For many people living with migraine, physical activity feels like a double-edged sword. Doctors recommend exercise for prevention, yet countless patients report that a workout can trigger an attack. This contradiction has led to years of confusion, fear of movement, and inconsistent advice.
So what does science actually say about physical activity and migraine?
Over the last two decades, large observational studies and clinical trials have started to clarify this paradox. The answer is not whether exercise is good or bad for migraine, but how, when, and at what intensity the brain is exposed to physical stress.
The Migraine–Exercise Paradox
Population-level data consistently show that people with low physical activity levels experience migraines more often. Sedentary individuals have higher migraine prevalence, increased attack frequency, and greater disability compared to those who move regularly.
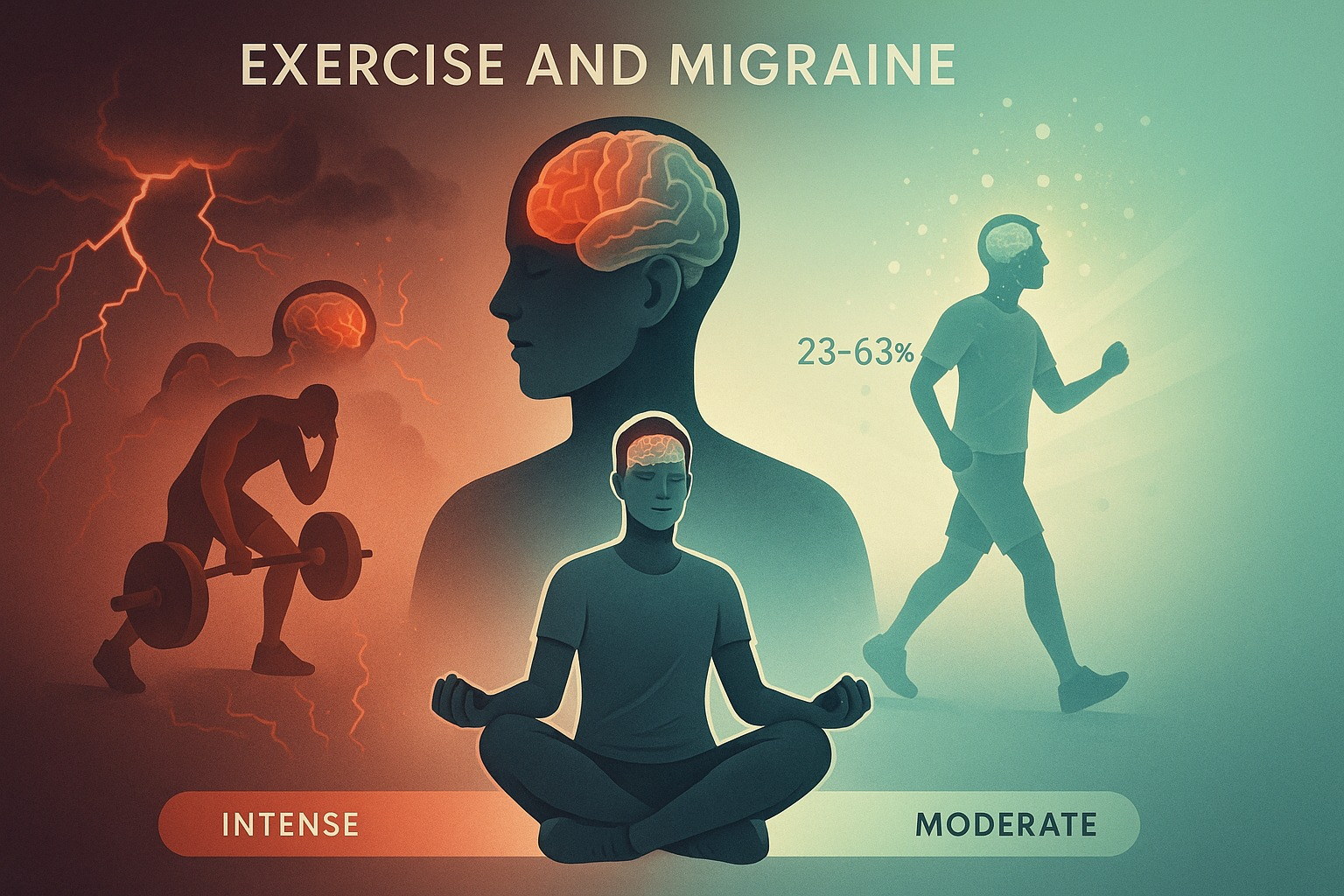
At the same time, intense or sudden physical exertion is a well-known trigger. Studies report that 9–57% of migraine patients experience attacks provoked by exercise, particularly when intensity rises abruptly or when other stressors are present.
At first glance, these findings seem contradictory. In reality, they describe two different physiological processes acting on the same vulnerable nervous system.
Why Inactivity Increases Migraine Frequency
Migraine is not simply a headache disorder. It is a condition involving impaired pain modulation, altered sensory processing, and dysregulated stress responses.
When physical activity is chronically low, several protective systems become weaker. Endogenous pain inhibition declines, autonomic balance shifts toward chronic stress activation, and the brain becomes less resilient to internal and external stimuli.
In other words, lack of movement lowers the migraine threshold over time. The brain becomes more sensitive, not less. This helps explain why sedentary lifestyles are consistently associated with higher migraine prevalence in epidemiological studies.
Why Intense Exercise Can Trigger Attacks
On the other hand, migraine is a classic threshold disorder. The migraine brain struggles with rapid changes.
Sudden high-intensity exercise can produce abrupt shifts in blood pressure, cerebral blood flow, metabolic demand, and cortical excitability. For a nervous system already prone to sensory overload, this rapid escalation can push neural networks beyond their adaptive capacity.
This is why many patients report that exercise is helpful in general, but a specific workout triggered an attack. The problem is not movement itself, but how quickly and aggressively the system is challenged.
This distinction is critical and often missing from generic lifestyle advice.
What Controlled Studies Reveal
Clinical trials offer a clearer picture of how physical activity can be used therapeutically.
When migraine patients engage in regular, moderate aerobic exercise, attack frequency decreases by approximately 23–63%, depending on the study and baseline migraine severity. These reductions are comparable to some preventive medications, without pharmacological side effects.
The most consistently effective pattern involves moderate-intensity activity performed several times per week, rather than sporadic or extreme efforts. Importantly, the benefits appear gradually, reinforcing the idea that migraine prevention depends on neural adaptation over time, not short-term exertion.
The Biological Mechanisms Behind the Benefit
One key mechanism is the increase in beta-endorphins following regular aerobic exercise. Beta-endorphins act as natural pain modulators and are often deficient or dysregulated in migraine patients. By enhancing endogenous pain control, exercise helps stabilize pain-processing pathways.
Another important factor is the rise in endocannabinoids after sustained moderate activity. These molecules reduce neuroinflammation, improve emotional regulation, and promote nervous system stability – all highly relevant to migraine pathophysiology.
Over time, regular exercise also improves autonomic nervous system balance, reducing chronic sympathetic overactivation that is frequently observed in migraine disorders.
Why Patterns Matter More Than Motivation
One of the most challenging aspects of migraine management is that triggers are rarely isolated. Exercise interacts with sleep, hydration, stress, hormonal state, and medication use. A workout that is well tolerated one day may provoke symptoms on another.
This is where pattern recognition becomes essential. Understanding which combinations of intensity, timing, and context are safe requires more than memory or intuition.
This is precisely why structured tracking is so valuable. By logging activity alongside symptoms, sleep, and recovery, people can identify personal thresholds rather than relying on generic advice. Tools like Hope & Mo are designed to make these relationships visible over time, helping users distinguish between preventive movement and trigger patterns based on real data rather than guesswork.
You can explore how this approach works in practice at
https://hopeandmo.com
Reframing Exercise in Migraine Care
The emerging scientific consensus does not support avoiding exercise. Instead, it suggests reframing movement as a dose-dependent intervention.
Regular, moderate activity trains the nervous system to become more resilient. Sudden or excessive exertion, especially without preparation or recovery, overwhelms it. The difference lies not in willpower or fitness, but in respecting the unique sensitivity of the migraine brain.
This perspective helps explain why fear-based avoidance often worsens migraine over time, while carefully structured activity can become one of the most effective non-pharmacological preventive strategies available.
Summary: Key Points to Remember
Migraine and exercise are not opposites. Low physical activity is associated with higher migraine frequency, while regular moderate aerobic exercise significantly reduces attacks. The problem arises when intensity increases too quickly or exceeds the brain’s adaptive capacity.
Migraine-safe movement is about consistency, gradual progression, and awareness of early warning signs. When activity is tracked alongside symptoms and recovery, exercise shifts from a source of uncertainty to a powerful preventive tool.
Regular moderate exercise supports migraine prevention. Sudden intense exertion can act as a trigger. Understanding the difference changes everything.